Specific Learning Objectives
- Functional Anatomy of Kidney
- JG apparatus
- Peculiarities of Renal Blood Flow
- Regulation of Renal Blood Flow
Location:
- A pair of kidney is located on either side of the vertebral column at the level of T12 to L3 vertebral column retroperitoneally.
- The kidneys are bean shaped structure with reddish brown in colour, weighs 150g each and measures 10 cm x 5 cm x 2.5 cm.
Surface, Borders & Poles of Kidneys
- There are 2 surfaces, anterior and posterior, 2 margins: medial and lateral and 2 poles: superior and inferior.
- Lateral margin is convex and medial margin is concave in which renal sinus and renal pelvis are located.
Renal hilum
- It is a vertical slit on concave medial margin and forms the entrance to renal sinus (space within kidney).
Renal sinus
- It consists of renal pelvis, calyces, vessels and nerves.
Renal pelvis
- It is the flattened, funnel-shaped expansion of superior end of ureter.
Renal calyces
- Within the renal sinus, pelvis divides into major calyces.
- Each major calyx divides into many of minor calyces.
- Each minor calyx fits into renal papilla (apex of the renal pyramid).
Kidney consists of outer cortex and inner medulla
1) Medulla
- It is made up of triangular areas of renal tissue called renal pyramids.
- There are around 4 -14 renal pyramids in each kidney.
- The base of pyramid is directed towards the cortex and the apex towards the pelvis which fits into the minor calyx.
- Pyramids show striations because of long nephrons running parallel giving appearance of medullary ray.
2) Cortex
- It is the area between the base of the pyramids and the capsule of the kidney.
- It consists of nephrons and blood vessels.
Microscopy of Kidney
Cortex and medulla consists of nephrons and blood vessels.
Nephrons
- They are the structural and functional unit of kidney.
- There are about 1.2 million in each kidney.
- All of them capable for forming urine.
Structure of a Nephron
A nephron consists of two major parts
- Renal corpuscle
- Renal tubule
1) Renal corpuscle
- It is also called as Malpighian corpuscle.
- It is a rounded structure consisting of glomerulus surrounded by glomerular capsule.
Glomerulus
- It consists of round tuft of anastomosing capillaries, diameter of 200 μm.
- Blood flows into the glomerulus via afferent arteriole and exit via efferent arteriole.
- It is also known as Bowman’s capsule.
- It encloses the glomerulus.
- It is formed of two layers:
- Inner layer covering the glomerular capillaries - Visceral layer
- Outer layer - Parietal layer
- It is a cup shaped structure at the beginning of the renal tubule.
- Bowman’s space (urinary space) is the space between visceral and parietal layer which is continuous with lumen of the renal tubule.
Ultrastructure of Glomerular membrane
It is the membrane which separates the blood of glomerular
capillaries from the fluid present in the Bowman’s space.
It is also called filtration barrier.
It consists of three major layers:
- Capillary endothelium
- Basement membrane
- Bowman’s visceral epithelium
- It is fenestrated with pores of diameter 70-90 nm.
- It is freely permeable to water, small solutes and small proteins.
(2) Basement membrane
- It is a matrix of glycoproteins and mucopolysaccharides.
- No pores are present here.
(3) Bowman’s visceral epithelium
- It forms the 3rd layer of the filteration membrane.
- It is formed by special cells called podocytes.
- Podocytes have finger-like processes which encircle the outer surface of the capillaries.
- The processes of podocytes interdigitate to cover the basement membrane, separated by gaps which are called as filtration slits with diameter of 25nm.
Mesangium
It is present between the capillary endothelial cells and
the basement membrane.
It consists of mesangium cells.
Function of Mesangium:
- Provide structural support for the glomerular capillaries.
- Secrete the extracellular matrix.
- Exhibit phagocytic activity.
2) Renal tubule
Renal tubule is divided into following parts
- Proximal tubule
- Loop of Henle
- Distal convoluted tubule
- Collecting duct
 |
| Parts of a Nephron |
1. Proximal tubule
It is divided into initial part which is convoluted, hence
called proximal convoluted tubule (PCT) followed by a straight part called
proximal straight tubule (PST) or pars recta that descends downwards into the
medulla.
2) Loop of Henle or Intermediate tubule
It consists of
- Descending thin segment (DTS)
- Ascending thin segment (ATS)
- Thick ascending limb (TAL)
3) Distal convoluted tubule (DCT)
It is the continuation of Thick ascending limb. Like the
proximal convoluted tubule, it is also convoluted.
4) Collecting duct
DCT continues as collecting duct
It is divided into three parts
- Cortical collecting duct (CCD: portion present in the cortex
- Outer medullary collecting duct (OMCD): portion present in the outer medulla
- Inner medullary collecting duct (IMCD): portion present in the inner medulla.
Several IMCDs coalesce together before finally opening at the
tip of the renal papilla
Characteristics of epithelium lining the renal tubule
Different segments of renal tubule have different type of epithelial lining.
These cells have special characteristic feature to perform specific transport functions.
Type of cells
The epithelial lining of renal tubule is mostly cuboidal
except in thin segment which has flat or squamous type of cells
The cells have 3 borders - apical surface, basolateral membrane and lateral surface
Apical surface of cuboidal cells of proximal convoluted tubule have microvilli which forms the brush border.
Basolateral membrane of PCT, TAS, DCT is highly invaginated and contains many mitochondria where as that of Descending and Ascending thin limb of Loop of Henle is poorly developed.
Lateral surfaces of the cells bear process which interdigitate with that of the adjacent cells.
Lateral surfaces of the cells form two types of tight
junctions
- Leaky tight juctions (present in PCT), they permit water and solutes to diffuse across them
- Tight tight junctions (present in DCT), they do not permit water and solutes to diffuse across them easily
Cortical collecting duct consists of two types of cells
- Principal cells (P cells): They are involved in Na+ absorption and also antidiuretic (vasopressin) stimulated water reabsorption.
- Intercalated cells (Ic cells): They are concerned with acid secretion and HCO3 absorption.
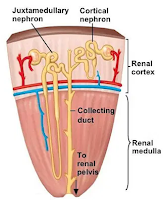
Types of Nephrons
There are two types of nephrons:
- Cortical nephrons (Superficial)
- Juxtamedullary nephrons
Juxtaglomerular apparatus (JG apparatus)
It is a collection of specialized cells near the glomerulus.
It forms the major component of
Renin–Angiotensin–Aldosterone system
It consists of 3 types of cells:
- Juxtaglomerular cells
- Macula densa cells
- Mesangial cells
1) Juxtaglomerular cells
- Specialised myoepithelial cells located in the tunica media of the afferent arteriole.
Function:
- They Synthesize, store and release of Renin which are stored in the secretory granules, hence they are also called as Granular cells.
- They act as baroreceptors: they respond to change in pressure gradient between afferent arterioles and interstitium.
- They are densely innervated by sympathetic nerve fibres, release renin in response to sympathetic stimulation.
- Monitor renal perfusion pressure.
2) Macula densa cells
- They are Specialized renal tubular epithelial cells of Thick Ascending Limb of loop of Henle.
- They are in direct contact with the mesangial cells.
- They act as chemoreceptors and are stimulated by decreased NaCl concentration in tubular fluid which causes increased Renin release.
3) Mesangial cells or lacis cells
- They are the Interstitial cells of the JG apparatus
- They are in contact with both macula densa cells and JG cells
- Structurally they are supporting cells.
- Functionally they relay the signals from macula densa to granular cells.
- Also secrete various substances that make up immune complexes.
Renal Blood Flow
Characteristics of renal blood flow
- Rate of renal blood flow is 1200 ml/min which is very high compared to other tissues.
- Total renal blood flow is 25% of cardiac output.
- Range of blood flow: has less reserve compared to other organs.
- Higher blood flow is related to excretory function than metabolic function.
- Blood flow directly proportional to pressure difference between renal artery and renal vein and inversely proportional to resistance of the renal vasculature.
- During blood pressure changes, renal blood flow shows remarkable constancy due to autoregulation.
- During exercise there is shunting of blood from renal vessels to skeletal muscles.
Important to note about renal blood flow
- Low perfusion of medulla plays important role in urinary concentration mechanism.
- Hydrostatic pressure in glomerular capillaries is very high which is an important factor for formation of glomerular filtrate.
- Peritubular capillaries have very low hydrostatic pressure which facilitates reabsorptive function of PCT & DCT.
Regulation of renal blood flow
- Constriction of afferent arteriole decreases both RBF and GFR
- Dilatation of the afferent arteriole increases both RBF and GFR
- Constriction of efferent arteriole decreases RBF but increases GFR
- Dilatation of the efferent arteriole increases RBF but decreases GFR
Regulatory mechanisms of Renal Blood Flow
- Autoregulation
- Hormonal regulation and
- Nervous regulation
1) Autoregulation
RBF & GFR remains constant for wide range of pressure:
80-200 mmHg
It is done by changing renal vascular resistance via 2 mechanisms
- one that respond to change in arterial pressure (Myogenic)
- one that respond to change in NaCl conc. in tubule (Tubuloglomerular feedback)
a) Myogenic mechanism
Vascular smooth muscle contract when stretched
Renal arterial pressure raised in afferent arterioles
▼
Stretched
▼
Contract
▼
Increase in vascular resistance
▼
Maintains a constant RBF and GFR
b) Tubuloglomerular feedback
2) Hormonal regulation
Hormones that cause vasoconstriction and hence decrease in RBF
and GFR are:
- Norepinephrine
- Angiotensin II
- Endothelin
Hormones that cause vasodilatation and hence increase in RBF
and GFR are:
- Prostaglandins
- Nitric oxide (NO)
- Bradykinin
- Atrial natriuretic peptide (ANP)
- Glucocorticoids
- Dopamine
3) Nervous regulation
Afferent and efferent arterioles are innervated by
sympathetic fibres from T10 to L2 segments.
Under normal circulatory conditions
- Sympathetic tone is minimum and no effect is seen.
Mild to moderate stimulation
- Mild effects on RBF because of autoregulation
Strong acute stimulation
- There is marked fall in RBF due to constriction both afferent and efferent arterioles (mediated through α1 adrenergic receptors than α2)
Summary
Functional Anatomy of Kidney
- Nephron – structural and functional unit of kidney
- Parts of nephron and cells lining the tubule
- Glomerulus
- Filtration membrane
- Types of nephrons
JG apparatus
- Cells of JG apparatus
- Hormones secreted
Renal Blood flow
- Characteristic features
- Regulation
- Autoregulation
- Hormonal
- Neural